Francesco M. Labricciosa, MD, Specialist in Hygiene and Preventive Medicine

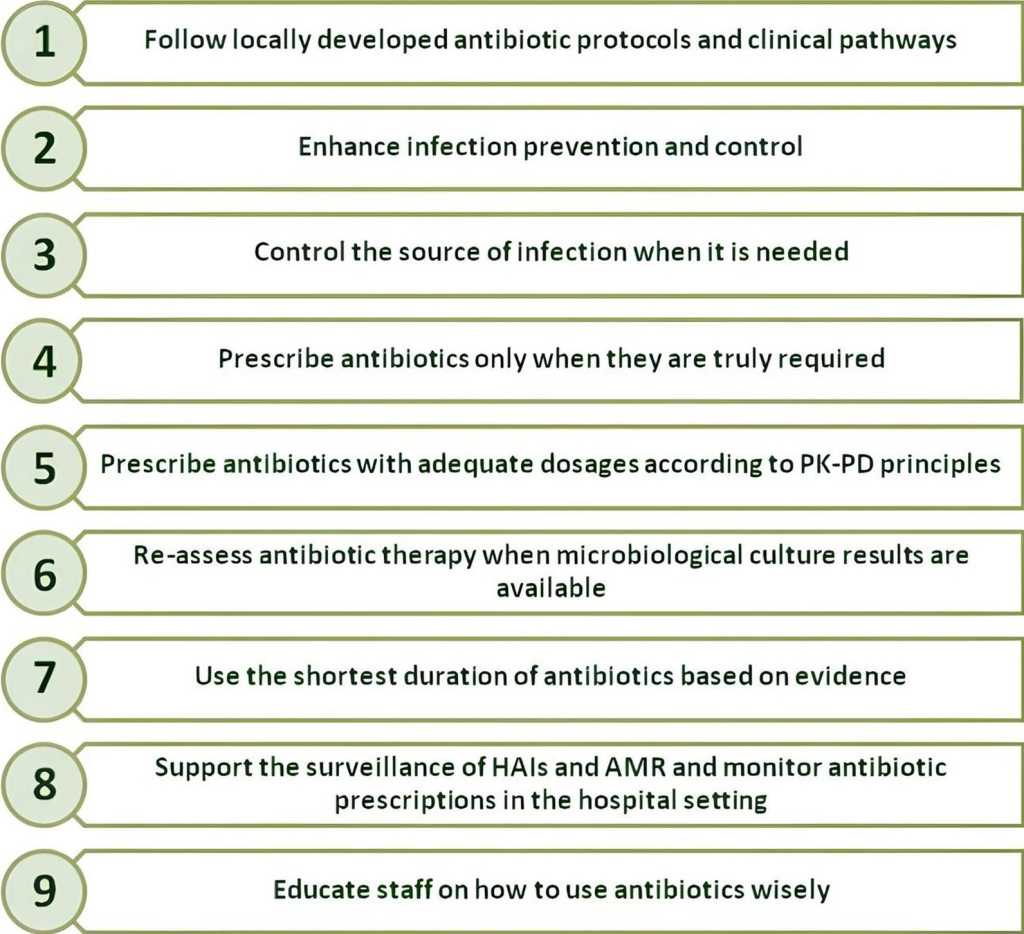
The misuse and overuse of antimicrobials are among the main drivers in the development of drug-resistant pathogens, and the appropriate use of these precious medications is paramount to preserve them for future generations to come. However, healthcare professionals should always keep in mind that also an inadequate infection prevention and control contributes considerably to the emergence and spread of antimicrobial resistance (AMR).
AMR is closely related to healthcare-associated infections (HAIs): the management of patients with HAIs frequently requires the administration of broader spectrum antibiotic regimens due to the higher risk of acquiring multidrug-resistant organisms. For this reason, even before using antimicrobials correctly, preventing the occurrence and controlling the spread of HAIs in healthcare facilities is essential. It should be considered the first principle of an appropriate antimicrobial stewardship program in every hospital worldwide.
In a paper recently published in Antibiotics, an international working group of physicians defined the most important measures to prevent and control HAIs in hospital settings.
In this narrative review, the authors presented seven measures that all healthcare workers must know and support. They focused their attention not only on the pivotal role of hand hygiene and the prevention of HAIs, but also on the importance of an effective environmental hospital hygiene, the implementation of surveillance systems, and patients’ screening, decolonization, isolation and cohorting. Finally, they did not forget to discuss about adapting evidence-based practices to the local context, and promoting safety culture.
The authors hope that this document can contribute to raise awareness among healthcare professionals about all issues associated with HAIs, and the need to embrace a personal involvement in the strategies that can help reduce their occurrence.
Fewer microorganisms there will be in our hospitals, fewer antimicrobials we will use. Fewer HAIs will develop in our hospitals, fewer broad-spectrum antibiotics we will have to use to combat multidrug-resistant organisms.