Francesco M. Labricciosa, MD, Specialist in Hygiene and Preventive Medicine

An interesting article has been recently published in the World Journal of Emergency Surgery. An evidence-based position statement signed by a multidisciplinary working group of experts, whose main objective was to describe the best practices for complicated intra-abdominal infections (IAIs) management.
The working group, representing the Global Alliance for Infections in Surgery, included physicians from several different disciplines: general and emergency surgeons, intensive care specialists, and infectious diseases specialists.
A comprehensive literature search of pertinent scientific evidence was performed using PubMed and Google Scholar, and articles published in English between January 2010 and December 2023 were identified to formulate 28 statements. Evidence quality has been graded high, moderate, low, or very low according to the GRADE methodology. For each statement, consensus among the experts was reached using a Delphi approach. Statements were endorsed as a strong recommendation with agreement by ≥ 80% of participating experts. The final document was approved by each working group member to ensure consensus.
Several factors of importance in the management of complicated IAIs were listed.
First of all, the origin of the infection must be taken into account. Indeed, the term “intra-abdominal infections” includes several different pathologic conditions ranging in severity from uncomplicated appendicitis to diffuse faecal peritonitis. The origin of the infection should be always investigated for treatment planning. Achievement of source control is of utmost importance in the management of complicated IAIs.
Assessing the anatomic extent of infection is equally important to define the treatment approach. In uncomplicated IAIs, the infectious process only involves a single organ, while in complicated IAIs, it extends beyond, into the peritoneal cavity, leading to abscess formation or diffuse peritonitis. This classification does not describe patients’ complexity, but in its simplicity, defining the extension of the infectious process identifies those patients who need both source control and antimicrobial therapy.
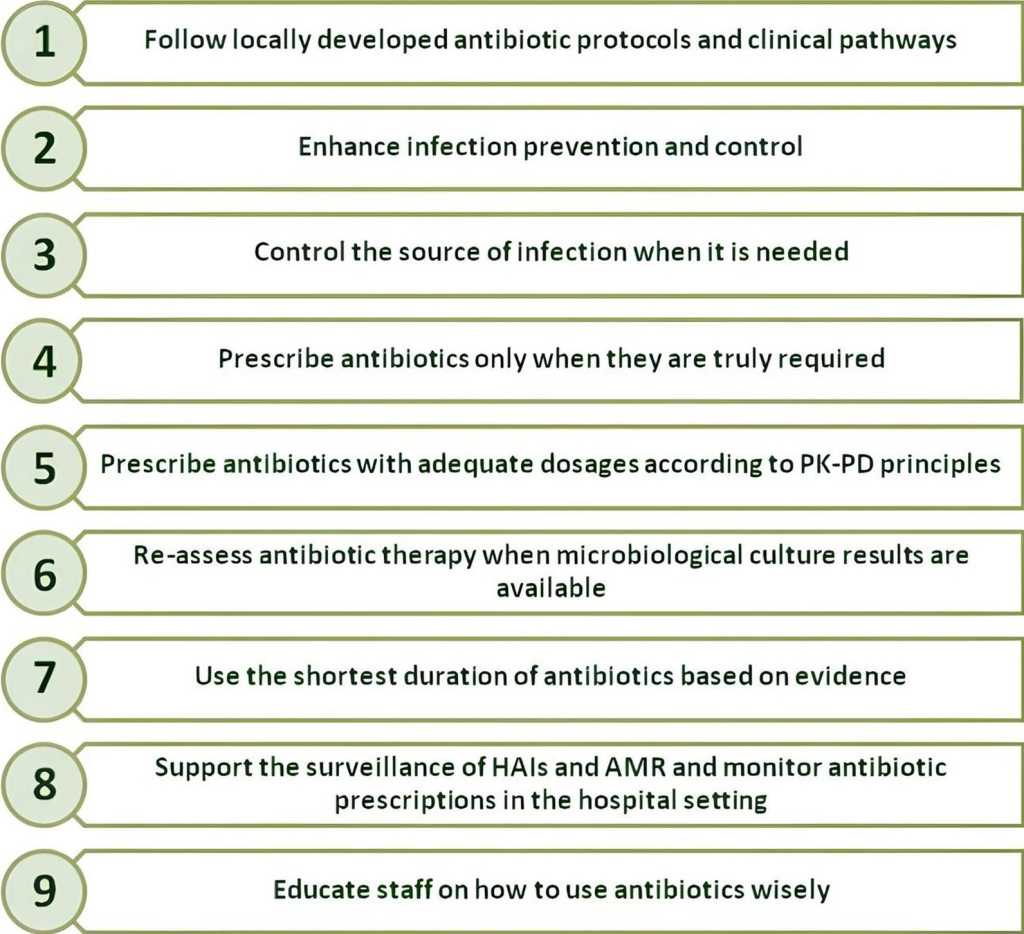
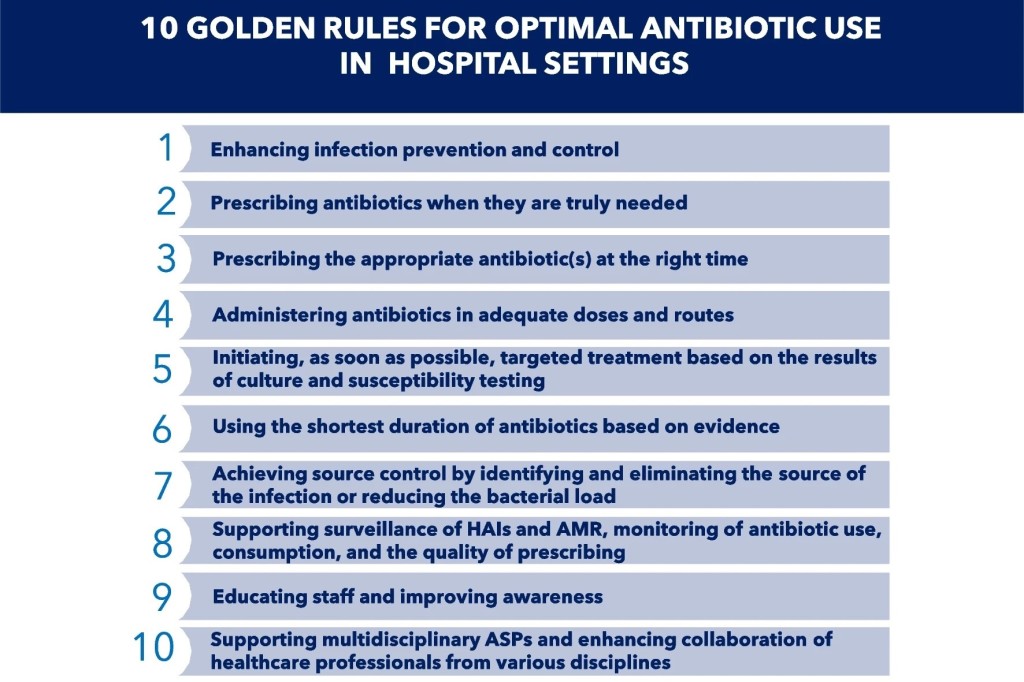
Moreover, taking into account presumed pathogens involved and risk factors for antimicrobial resistance is crucial. Initial antimicrobial therapy for complicated IAIs is typically empiric in nature because standard microbiologic data and susceptibility results generally require 24-72 hours after peritoneal fluid specimen collection. For these reasons, an accurate patient stratification is crucial to optimize empiric antimicrobial therapy.
Finally, clinical conditions and host immune status have to be carefully considered when managing a patient with a complicated IAI.
The authors concluded that complicated IAIs are conditions sometimes difficult to manage, and available treatment options should be always assessed to optimize the management of patients with complicated IAIs.