Francesco M. Labricciosa, MD, Specialist in Hygiene and Preventive Medicine

Necrotizing soft tissue infections (NSTIs) are acute and rapidly progressive infections, resulting in extensive tissue destruction due to the production of toxins which cause tissue damage, ischemia and necrosis. Consequently, NSTIs are often associated with signs of severe systemic toxicity and progressive multiorgan failure.
An early diagnosis – based on clinical evaluation, laboratory and radiological tests – together with a prompt surgical intervention, and an appropriate antibiotic treatment are essential elements to reduce mortality and improve outcomes.
However, despite important advances in critical care medicine over the last few decades, the mortality rate is still high, and survivors are at a significant risk of long-term morbidity. Indeed, after a prolonged hospitalization, multiple dressing changes and surgical procedures, the survivors have to face continued physical therapy to regain functional independence. A multidisciplinary approach should focus not only on survival but also on long-term functional outcomes.
In a paper recently e-published (ahead-of-print) in the Journal of Trauma and Acute Care Surgery, Massimo Sartelli, together with an international and multidisciplinary research group of physicians, signed an evidence-based position statement, whose main objective was to describe the best practices for the first-line management of NSTIs in adult patients.
The working group, representing the Global Alliance for Infections in Surgery, included physicians from several different disciplines: general and emergency surgeons, intensive care specialists, and infectious diseases specialists.
A comprehensive literature search of pertinent documentation was performed using PubMed and Google Scholar, and articles published in English between January 2010 and August 2024 were identified. Evidence quality has been graded high, moderate, low, or very low according to the GRADE methodology. The strength of the recommendations has been classified as weak or strong. The final document was approved by each member to ensure consensus.
First of all, the authors declare that a multidisciplinary collaboration is mandatory for the first-line management of NSTIs. Diagnosis should be made as soon as possible. Due to the quick progression of the inflammatory process, a rapidly progressive soft-tissue infection should always raise suspicion of NSTI.
Early source control is one of the cornerstones of treatment in patients with NSTIs. Surgical debridement with complete removal of necrotic tissue is essential to decrease mortality and other complications, and should be performed as soon as possible within 6 hours after presentation, supporting the concept that earlier surgery is performed, better is the outcome.
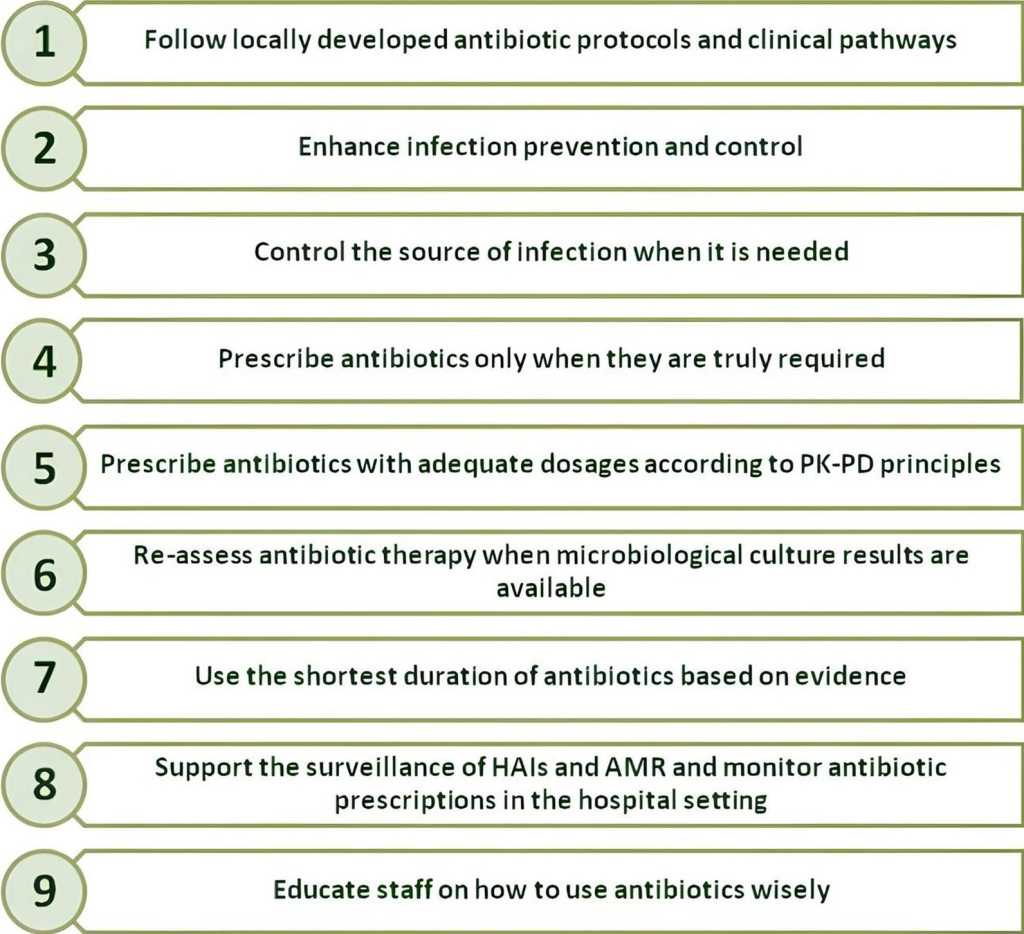
Moreover, antibiotic treatment and supportive treatment in managing NSTIs must be prompt and aggressive to halt the progression of the inflammatory process. Post-operative wound care and along-term and multidisciplinary management of the patient must always be considered. Finally, a conclusive section is dedicated to Fournier’s gangrene.
The authors conclude that public health policies promoting education among both healthcare providers and patients, and expert centres, together with systematic data collection could lead to better outcomes for NSTIs in the future.
Reference