Francesco M. Labricciosa, MD, Specialist in Hygiene and Preventive Medicine

Antimicrobial resistance (AMR) represents a serious threat to global health because antibiotics are losing effectiveness in both prevention and treatment of infections. The rising incidence of multidrug-resistant organisms (MDROs) challenges the efficacy of conventional surgical antibiotic prophylaxis (SAP) regimens.
Addressing this issue requires a re-examination of perioperative protocols, with attention to individual patient risk factors for MDRO colonization. Therefore, a targeted SAP approach should be considered when MDROs represent a significant surgical site infection risk. Thus far, limited evidence provides guidance on SAP selection in high-risk patients.
For these reasons, a position paper has been recently publishedin Pathogens by the Italian Multidisciplinary Society for the Prevention of Healthcare-Associated Infections (SIMPIOS). Following the best scientific evidence from PubMed and EMBASE Library a multidisciplinary working group produced 15 recommendation statements to optimize SAP in a context of AMR. They were graded according to the GRADE hierarchy of evidence. Using a Delphi approach, statements reaching ≥80% agreement were approved as strong recommendations.
This position paper is structured in three sections.
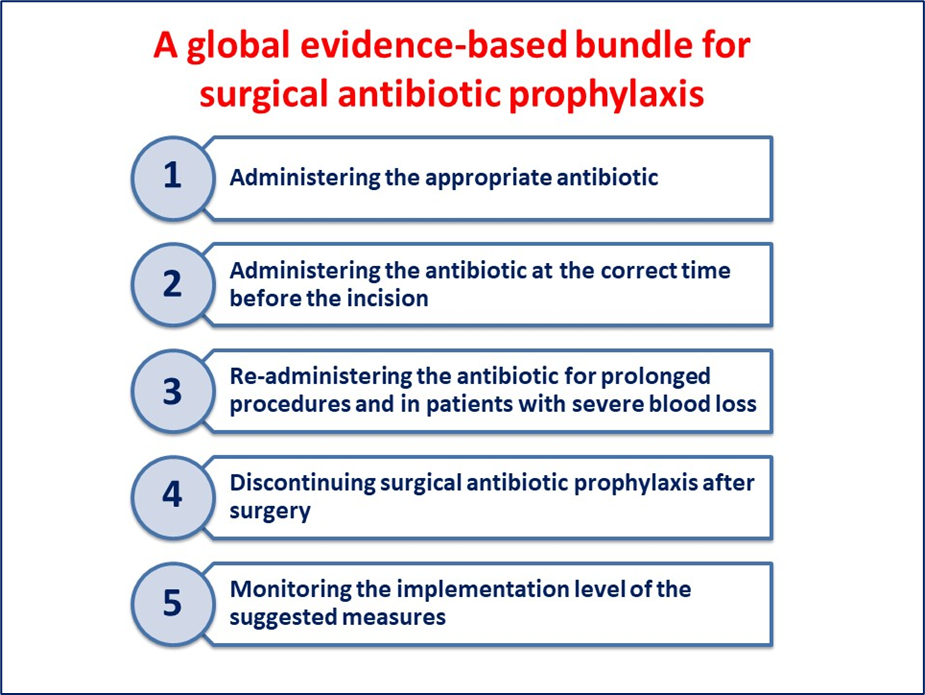
The first one widely reviewed the core principles for appropriate SAP. Then, the second section examined screening, decolonization, and targeted SAP in patients colonized with MDROs focusing separately on Gram-positive bacteria (methicillin-resistant Staphylococcus aureus [MRSA] and vancomycin-resistant enterococci [VRE]), and Gram-negative bacteria (extended-spectrum beta-lactamase [ESBL]-producing and carbapenem-resistant Enterobacterales [CRE]).
The third section discussed the barriers to changing surgeons’ prescribing behaviours, focusing on surgeons’ awareness and dynamics within surgical teams that influence antibiotic prescribing practices. To track adherence and improvement in SAP, the authors listed the key performance indicators, and suggested a checklist, too.
Finally, they summarized all the 15 recommendation statements expressed by the multidisciplinary working group in order to provide practical guidance for optimising SAP in the context of an AMR era.
The authors concluded that in the AMR era the goal is to ensure that SAP remains effective in preventing infections while minimizing unnecessary antibiotic exposure. This can be achieved balancing patient safety with stewardship principles, tailoring SAP to epidemiological risk, and promoting a culture of shared responsibility across the surgical pathway.
Reference